Tuberculosis (TB): Frequently Asked Questions
What is Tuberculosis?
Tuberculosis or "TB" is a disease caused by a bacterium (germ) called Mycobacterium tuberculosis. TB usually affects the lungs but it can also affect other parts of the body, including the glands, the bones and rarely the brain.
Tuberculosis used to be more common in Ireland. There were nearly 7000 cases a year in the early 1950s. The incidence of TB has declined steadily since then. Detailed reports on the epidemiology of TB in Ireland are available on the HPSC website. Doctors are obliged to notify each case of TB to the local Departments of Public Health in the Health Service Executive.
TB disease is preventable and curable.
What are the symptoms of TB?
Symptoms of TB can include any of the following:
- Fever and night sweats
- Cough (generally lasting more than 3 weeks)
- Weight loss
- Blood in the sputum (phlegm) at any time
A person with any of these symptoms should visit their family doctor for advice. If someone has a reason to think that they might have TB, they should tell this to their doctor.
How is TB spread?
TB is usually spread in the air from another person who has TB of the lungs. It is spread by that person coughing, sneezing or spitting. People with TB in the lungs or throat can be infectious. This means that the bacteria can be spread to other people. Even then close and prolonged contact with such a person (i.e. family, friends, childminder, co-worker, classmate) is needed to become infected. Most cases of infectious TB stop being infectious after a few weeks of treatment. TB in other parts of the body such as the kidney or spine is usually not infectious.
Another type of TB called Mycobacterium bovis can arise from drinking contaminated milk. This form of TB is now rare as pasteurisation of milk removes the risk.
The following people have a greater chance of becoming ill with TB, if exposed to it:
- Those in very close contact with infectious cases
- Children
- Elderly people
- People with diabetes
- People on steroids
- People on other drugs affecting the body's defence system
- People who are HIV positive
- People in overcrowded, poor housing
- People dependent on drugs or alcohol
- People with chronic poor health.
What happens when a person is found to have infectious TB?
- Treatment for TB is started
- Public health doctors talk to the infected patient to see if other people need to be checked for TB.
What is the difference between latent tuberculosis infection and active tuberculosis disease?
Infection with the TB bacterium may not develop into TB disease. Most people who are exposed to TB are able to overcome the bacteria. The bacteria become inactive, but they remain dormant (asleep) in the body and can become active later. This is called latent TB infection (LTBI).
People with latent TB infection:
- Have no symptoms
- Don't feel sick
- Can't spread TB to others
- Usually have a positive skin test reaction
- Can develop TB disease later in life.
Most people who have latent TB infection never develop active TB disease. In these people, the TB bacteria remain inactive for a lifetime without causing disease. But in some people, who have weak immune systems, the bacteria can become active and cause active TB disease.
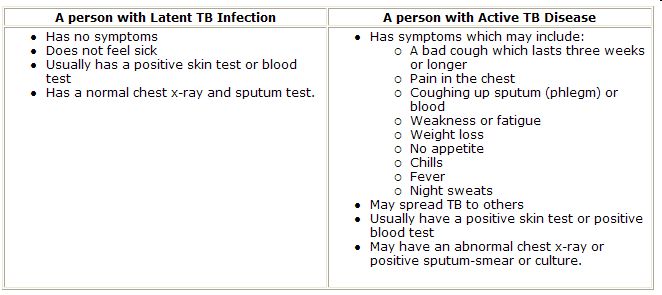
The Difference between Latent TB Infection and Active TB Disease
How is TB diagnosed?
All persons with the following symptoms should be checked for TB:
- Unexplained cough with or without phlegm (generally lasting more than 3 weeks) with at least one of the following symptoms:
- Fever
- Night sweats
- Loss of appetite
- Loss of weight for no reason
- Unusual sense of tiredness and felling unwell
- Coughing up blood
There are a number of tests that can be done to check for TB:
- A skin test (Mantoux test)
- A test of the sputum (phlegm)
- A chest X-ray
- A blood test (IGRA)
- A test of the urine
How is TB treated?
Today, TB is potentially completely curable, if the responsible organism is fully sensitive to the antibiotics being used and the patient takes his or her medication as prescribed.
TB is treated with tablets, which must be taken for at least six months. Without treatment, many people in Ireland used to die from TB. It is essential to take the treatment regularly and to complete the course as prescribed.
The most common medicines used to treat TB are: isoniazid, rifampicin, ethambutol and pyrazinamide. A vitamin B6 tablet called pyridoxine is also prescribed to help prevent some of the side effects that may be caused by isoniazid. Your specialist doctor will decide which TB drugs are best for you.
If you have infectious TB (TB disease of the lungs or throat), you will need to stay at home from work or school so that you don’t spread the TB bacteria to other people. After taking your medicines for a few weeks, you will feel better and will no longer be infectious to others. Your doctor will tell you when you can return to work or school or visit friends.
What are the side effects of TB medicines?
If you are taking medicines for TB, you should take them as directed by your doctor or nurse. The medicines may cause side effects but everyone can react differently and not everyone will have the side effects. It is important to report any side effects to your doctor even if they are not listed below. Side effects include:
- No appetite
- Nausea (feeling sick in the stomach) and/or vomiting
- Abdominal pain (tummy pain)
- Yellowish skin or eyes
- Dark-coloured urine
- Fever for 3 or more days
- Skin rash
- Itching
- Tingling of fingers or toes or around the mouth
- Easy bleeding and/or bruising
- Blurred or changed vision
- Ringing in the ears
- Hearing loss
- Dizziness
- Aching joints
The following side effects are caused by rifampicin. If you have any of these side effects you can continue your medications (your doctor will advise you of these before starting treatment for TB):
Rifampicin can:
- Turn your urine, saliva (spit) or tears orange. The doctor or nurse will advise you not to wear contact lenses as they may get stained.
- Make your skin more sensitive to the sun. This means you should use a good sunscreen and cover exposed areas so that they don’t burn.
- Make birth control pills and implants less effective. Women who take rifampicin should use another form of birth control
How important is treatment?
Treatment is very important. If you have TB disease or if you have been infected with the TB bacterium but have not yet become unwell i.e. have latent TB infection, you must take the treatment as directed. It is very important to complete the full course of treatment as it will stop you being infectious (spreading the disease to others) and it will remove the risk of you developing drug-resistant TB. It is important to remember that TB used to kill people before we had modern treatments.
Can I drink alcohol with my medication?
It is always best to avoid alcohol while you are taking TB medicines. This is because drinking any alcohol can increase the chances of having problems with your liver when taking the medications.
What precautions need to be taken to prevent TB spreading in the home?
Some patients who are infectious (with TB) can remain at home in the household that has already been exposed. However the following precautions should be taken:
- Use tissues when sneezing or coughing and place into a household bin immediately after use
- Wash hands after disposing of the tissues
- Stay at home and not go to places where there will be previously unexposed people (e.g. pubs, clubs, cinemas)
- Attend all outpatient visits
- No visits by previously unexposed people
- Children who do not live at home should not visit until your doctor allows
- Relatives or friends who are immunosuppressed should not visit until your doctor allows
- You can go for a walk outside but you should avoid close contact with previously unexposed people
Most people are no longer infectious when they have completed a few weeks of TB tablets and are feeling better and their cough is gone or improving. However your doctor will advise you when the above precautions are no longer necessary. It is also very important that you continue your medications until the doctor tells you to stop.
What should I do, if I have been in contact with someone with TB?
The local Director of Public Health should be notified of all cases of TB. This is usually done by the patient’s doctor. Once local public health is notified of a case of TB, they will assess the risk of TB to people who were in contact with the person who has TB. Only close contacts are at risk of catching TB. Once the public health doctors have assessed this risk, they will decide which persons in contact with the case need to be tested for TB.
If you need to be tested for TB, you will be asked to attend a chest or contact tracing clinic, and to have a skin test and/or a chest X-ray. A public health doctor or nurse will contact you first (they will have a list of close contacts of the person who has TB). This does not necessarily mean that you have TB, but is a chance to check for it, so it is very important to attend if you are asked to. If you are unsure about anything relating to the TB testing, you may discuss this with the public health doctor.
Can TB be prevented?
Yes it can in several ways:
- Most important is early detection, especially of infectious cases, and complete treatment: Early case detection reduces onward transmission of the disease and a full course of treatment is vital to prevent the disease relapsing, to prevent the development of drug-resistant strains of TB and to prevent prolonged infectiousness.
- Treating all people with active TB disease promptly. After two weeks of treatment, most patients are no longer infectious to other people.
- Ensuring that all close contacts of people with TB are seen promptly in the chest or contact tracing clinic. Those found to have latent TB infection or those at high risk of developing TB after close contact may be offered a course of preventive therapy (chemoprophylaxis) once active TB has been ruled out.
What happens if I don’t complete TB treatment?
Your TB infection may relapse and become much more difficult to treat, due to the TB bacteria becoming resistant to the antibiotics which were taken for too short a time. Also, if you are infectious to others, they may also become infected with resistant TB. See information on MDR-TB and XDR-TB below.
What are Multidrug-resistant TB (MDR-TB) and Extensively drug-resistant TB (XDR-TB)?
Multidrug-resistant TB (MDR-TB)
MDR-TB is a specific form of TB which is resistant to at least isoniazid and rifampicin, two of the main first line drugs used in the treatment of TB. MDR-TB therefore is much more difficult to treat. It takes longer to treat with second line drugs which are more expensive and have more side-effects.
Extensively drug-resistant TB (XDR-TB)
XDR-TB is a rare type of MDR-TB which is also resistant to any of a group of drugs called fluoroquinolones and at least one of three injectable second line anti-TB drugs (capreomycin, kanamycin or amikacin). Because XDR-TB is resistant to first line and second line drugs, treatment options are more limited.
Further information on XDR-TB can be found on the WHO website at: https://www.who.int/news-room/questions-and-answers/item/tuberculosis-extensively-drug-resistant-tuberculosis-(XDR-TB)
WHO has prepared frequently asked questions on TB that is "resistant to all drugs": https://www.who.int/news-room/questions-and-answers/item/tuberculosis-multidrug-resistant-tuberculosis-(mdr-tb)
Information on TB in Ireland can be found on the Health Protection Surveillance Centre website
Information on BCG vaccine can be found in the Immunisation Guidelines for Ireland
Last updated: 21 March 2019


