Cold Weather Advice for Health and Care Professionals
Cold weather brings health risks, and it is important that health and care professionals remain cognisant of these for those they care for. Promoting vaccination against common winter viruses, including COVID-19, flu, and pneumococcus is an important preparatory step that can be performed in advance of cold weather and the increased risks of viral transmission that follow. Other risks over the winter months include the dangers of icy conditions and associated risks of falls and injury, cold-related illnesses including hypothermia and frostbite, and an increased risk of carbon monoxide exposure and poisoning. Further advice is available on the HSE website. In addition, Met Éireann provide up-to-date forecast information and issue warnings for predicted cold snaps. The Government’s Be Winter Ready campaign provides advice on how to prepare for winter that can be shared with the population you care for in advance of cold weather events. Hospital managers should support staff through the winter months by providing access to training and enabling capacity development to allow for safe and effective care delivery.
Those particularly vulnerable to cold weather include those:
- Over the age of 65,
- Under the age of 5,
- With chronic health problems such as cardiac, respiratory, or kidney disease
- With a disability,
- Who have dementia or memory problems,
- Experiencing homelessness and financial difficulties.
Keeping the Environment Warm
It is important to keep the environment warm to ensure that patients/clients do not suffer the adverse effects of low temperatures. Reduce draughts where possible and heat rooms to a comfortable temperature. The need, however, for reducing exposure to cold must be balanced with an ongoing requirement for good ventilation, given the increased risk or virus transmission. Re-iterate advice that people should take care when attending social gatherings and take visiting into consideration over the winter period. Consider adjusting individual patient care plans and/or increasing the frequency of monitoring of patient vital signs so that any exposure to cold can be identified early.
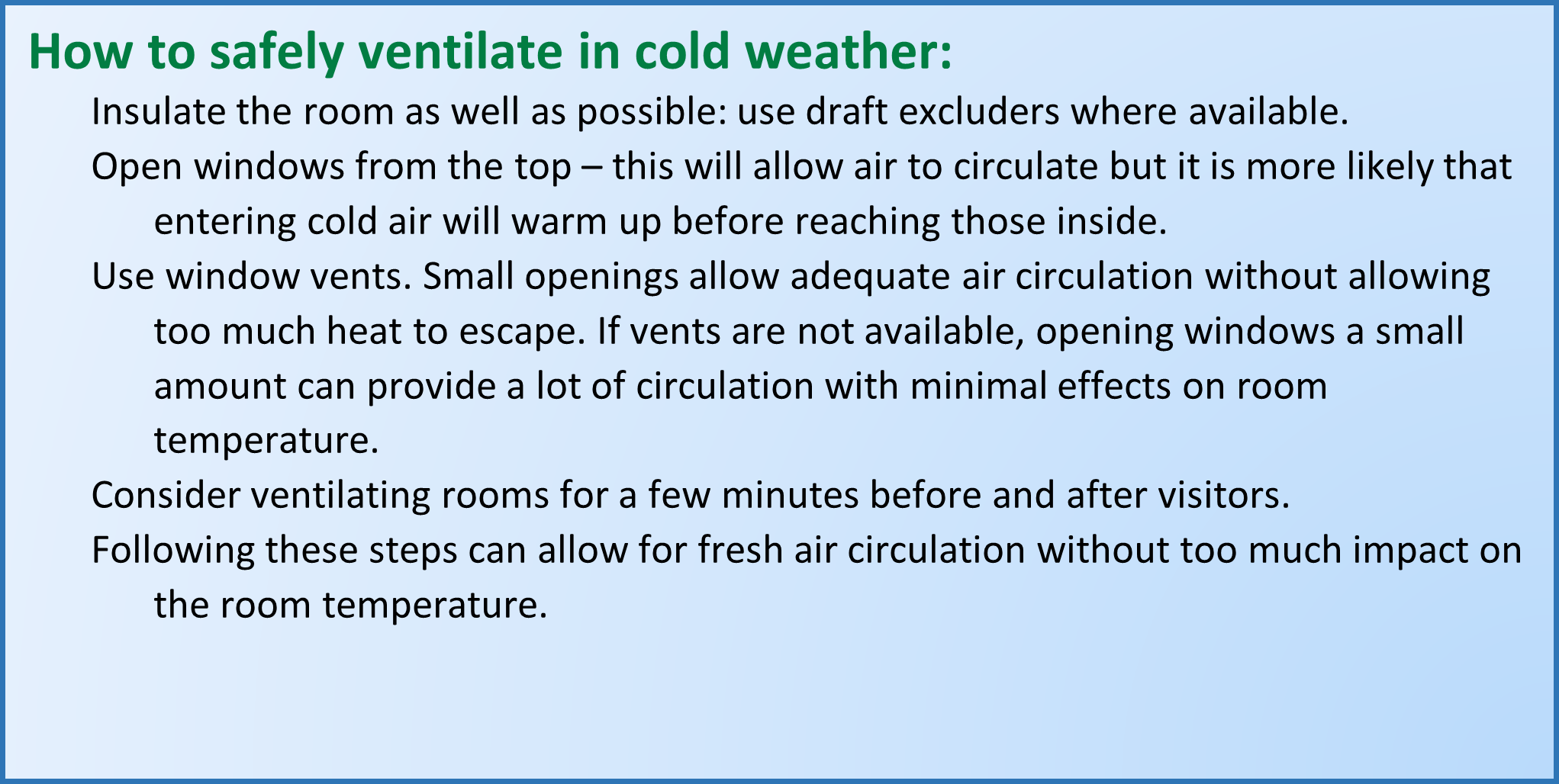
Safe Room Ventilation During Cold Weather
Effective ventilation remains important even when the temperatures are low. Fresh air circulation helps to reduce the risk of virus transmission. The guidance below details how to enable fresh air circulation whilst minimising exposure of patients/clients to low temperatures.
Hypothermia
Hypothermia is life-threatening and must be recognised immediately.
Hypothermia is defined as a core body temperature below 35°C. Signs of hypothermia include:
- Core body temperature < 35°C
- Cold skin in areas normally covered by clothing, for example, abdomen/axilla
- Shivering
- Drowsiness
- Slurred speech
- Slow breathing
- Confusion or disorientation
- Incoordination
- Thready pulse
Anyone with signs of hypothermia should undergo immediate medical review. Follow your facility protocol for the management of patients with hypothermia. Be aware that cardiac arrest can be more easily precipitated in hypothermic patients and therefore gentle handling of the patient is mandatory.
Advice for Patients with Specific Medical Conditions
Consider reaching out in advance to patients you care for in the community who may experience increased risks during cold weather. For example, those with chronic kidney disease, who are on dialysis therapy, may require changing of appointments if access routes are likely to be closed; ensure those with diabetes have access to insulin therapy and that they are aware that insulin may not work if it has frozen and thawed. Advise those with respiratory conditions, such as asthma, to ensure proper regular use of preventive inhalers and to keep relievers close to hand as cold weather may trigger asthma. Chest infections are also more common during the winter months. Those with cardiac disease should be reminded that strenuous activity, such as clearing snow, might place extra strain on their heart and that they should avoid this. Additionally, cold weather can increase the risk of clots and therefore of myocardial infarctions and cerebrovascular accidents/strokes. People with osteoporosis will need to take extra care in icy conditions as they will have a higher predisposition to fractures.
Safety Upon Patient Discharge
Discharge planning teams should take into consideration discharge destinations for patients to ensure that room temperatures will not expose a patient to hypothermia once they have left the hospital. A discussion with patients’ families may be appropriate to alert them to the potential for increased needs and risks during cold weather upon their discharge. For those with financial difficulties, who may find it difficult to heat their home, consider supports they may be entitled to in advance of discharge. These include:
- Vulnerable customer registers for the energy companies and Irish Water.
- Fuel allowance to help with the cost of heating during the winter months. Many people getting a social welfare payment will qualify for this allowance.
- In addition, an expanded fuel allowance scheme for those aged over 70 was introduced in 2022. Under this scheme, the means-tested threshold has been reduced, meaning that more people will now qualify for additional energy supports. Patients can apply for this scheme here.
- Patients may be entitled to a free or subsidised home energy upgrade through the SEAI.
Also consider those who reside in supported accommodation and that attending carers are aware of the potential increased needs and risks during cold weather. Also check that the patient has up-to-date contact information for their primary care GP should they require medical advice from the community.
Last updated: 4 January 2023


