Heat Health Advice for Health and Care Professionals
Service Preparedness for Warm Weather
Service providers who have a duty of care towards their clients, and those who work with vulnerable populations, need to be aware of the effects and additional demands placed on them during a heatwave. Heat stress, heat exhaustion and heatstroke are potentially serious health risks for people during a heatwave and deaths have occurred at home, in residential care facilities and in hospitals. Certain population groups are particularly vulnerable during heatwaves and suffer higher mortality rates. These groups include:
- Older people – especially those over 65 years of age
- Babies and children under 5 years of age
- Those who live on their own, and who may not be able to care for themselves, or are socially isolated
- Those living in a residential care facility
- People who have a serious or long-term health condition including heart, lung or kidney disease, diabetes, peripheral vascular disease, obesity, Parkinson’s disease, or some mental health conditions
- People taking medications that affect heart or kidney function, their ability to sweat, or their cognition or behaviourThose with behavioural limitations, such as people with cognitive impairment (dementia/Alzheimer’s), restricted mobility, or those with drug and/or alcohol addictions
- Those who are bed-bound, and those dependent on others for routine activities
- People with heightened exposure to heat, such as those who are experiencing homelessness and/or sleeping rough, people living in a top floor flat, those with outdoor occupations/activities
Service providers who deliver care for people within these more vulnerable groups therefore need to ensure that they deliver that care in a safe, temperature-controlled environment in order to protect clients or service users. The section “Health and Residential Care Facilities” below offers more detailed information for those working in health and care settings.
Target temperatures
- Room temperature should be about 20°C (18°C to 23°C comfortable range)
- Ideally, all patients – particularly those who are most vulnerable – should be cared for in a cool area, unless there is a clinical reason for this not to be the case.
Assessment and Action Plans
- Draw up a plan for measuring and monitoring temperatures throughout the day and night
- Identify places that are cool/comfortable (< 20°C)
- Identify places that have temperature problems that need to be addressed and aim to reduce these areas’ temperature to < 20°C
- Prioritise high-risk individuals to cooler areas
- Turn off unnecessary lights/electrical equipment
- Use curtains/blinds to keep sunlight out
- Use fans and/or air conditioning, where available and safe to do so
- Ensure sufficient on-site cool water and ice*
- Ensure sufficient staffing, and communicate heatwave plan to staff
- Recognise the signs of heat stress, heat exhaustion and heatstroke and act immediately if any of these are suspected. Heatstroke is a medical emergency and requires immediate medical help and calling 112/999 for an ambulance.
*Ice storage receptacles, ice making machines and water dispensers should be properly maintained and regularly cleaned. Ice and ice making machines may be contaminated through improper handling of ice by patients or staff.
Health and Residential Care Facilities
This section offers advice to those working in health and residential care settings.
Patients in hospital and residential care facilities are particularly vulnerable to extreme temperatures. Service providers should be aware of the actions needed to ensure the continued safe delivery of care during heatwaves. Careful preparation is required to ensure no excess heat-related morbidity or mortality, and plans should be in place before the start of the warm weather season each year. The National Health Protection Service of Ireland (NHPSI) works closely with Met Éireann to issue health alerts during times when the temperature poses a risk to health.
At-risk groups
Whilst extreme temperatures can be detrimental to the health of all individuals, certain populations are particularly vulnerable. In a healthcare facility setting these groups would include:
- Patients > 65 years of age
- Babies and children < 5 years of age
- Patients with long-term health conditions, particularly those with chronic cardiovascular and/or respiratory disease
- Patients taking medication that affects heart or kidney function, their ability to sweat or their behaviour or cognition
- Those with cognitive impairment, such as dementia
- Those with drug and/or alcohol addictions
- Patients who are bed-bound, and those dependent on others for routine activities
- Observe patients who are fasting for procedures or other reasons carefully
- Patients with vomiting/diarrhoea/anorexia will be at high-risk of dehydration
Actions
Having a plan prepared in advance will allow time for the additional training of staff in how to care for their patients during extreme weather events. The following actions should be carried out in order to ensure the environment is a safe temperature, identify those patients at highest risk of extreme temperatures, respond to unsafe indoor temperatures, and identify and respond immediately to any signs of severe heat-related illness like heatstroke.
- Draw up a plan for measuring and monitoring temperatures throughout the day and night – automatic temperature control is preferable, where available
- Identify places that are cool/comfortable (< 20°C)
- Identify places that have temperature problems that need to be addressed, and aim to reduce these areas’ temperature to < 20°C
- Prioritise high-risk patients to cooler areas, and monitor frequently
- Consider weighing patients regularly to assess for signs of dehydration
- Reschedule physiotherapy to cooler hours, where possible
- Turn off unnecessary lights/electrical equipment
- Use curtains/blinds to keep sunlight out
- Use fans and/or air conditioning, where available and it safe to do so
- Where air conditioning is used, keep windows closed to keep cooler air inside
- Ensure sufficient on-site cool water and ice*
- Ensure sufficient staffing to deal with any increased care needs
- Ensure staff are trained in any additional management strategies required during extreme temperature events, and communicate the action plans to staff
Hospital/Facility Management
It is important that hospital and facility management teams ensure business continuity and prepare for any potential surge in demand, balancing ability to provide additional capacity with the capability to provide safe and effective care. The following should be considered:
- Cooling the building at night
- Ensure discharge planning takes home temperatures and any additional support that may be required into account
- Liaise with infection prevention and control teams regarding the use of fans and air conditioning
- Ensure staff and patients have access to cooler areas
- Ensure adequate cold water and ice* is available
- Report any unforeseen or additional challenges to senior management so that any additional resources can be deployed
*Ice storage receptacles, ice making machines and water dispensers should be properly maintained and regularly cleaned. Ice and ice making machines may be contaminated through improper handling of ice by patients or staff.
Residential Care Settings
In addition to the above considerations, residential care homes should follow the below guidance.
Visit patients more regularly, where possible, to ensure they have ample opportunities to move to cooler areas, plenty of cool drinks available, and so that signs of dehydration can be adequately monitored.
Ensure availability of a cool room or area, that can be kept below 20°C, for residents to access whenever they need to cool down. High-risk groups can find it hard to cool themselves at temperatures above 26°C, and are particularly vulnerable to the effects of heat. Cool areas can be developed with appropriate indoor and outdoor shading, ventilation, the use of indoor and outdoor plants and, if necessary, air conditioning.
Ensure that patient rooms and common areas are temperature checked regularly, and high temperatures are responded to urgently. Keep curtains/blinds closed during the day to keep sunlight out – the use of reflective material can help. Avoid the use of metal venetian blinds and dark-coloured curtains, which will absorb heat. Turn off all unnecessary lights and electrical equipment. Open windows at night when the air is cooler, if it is safe to do so.
Visiting hours should be moved to morning time, if possible, as the air is cooler and heat will be generated by increased numbers of people inside.
For patients who either cannot be moved to cool areas, or who would find a move disorientating of distressing, cooling can be performed in the patient’s room. Use cool wipes or a damp cloth on exposed areas such as the back of the neck, ensure adequate hydration with cool liquids, and be vigilant in monitoring for signs of dehydration. Make sure the person is in lightweight, loose-fitting and light-coloured clothing, where possible. If going outside make sure they are wearing a high SPF sunscreen and light clothing that covers most sun-exposed areas.
Plastic pads and mattresses can make a person warmer – consider alternatives where available.
The use of electric fans can help with air circulation. Be careful when using electric fans to ensure compliance with infection control procedures. Do not point the electric fan directly at the person, as this can lead to dehydration. This is particularly important for people with reduced mobility.
Supply patients with a spray bottle with cold water, to help them keep themselves cool. Plan cool baths or showers, where feasible.
Monitoring for signs of dehydration is particularly important. Consider checking weight more regularly. Urine should be pale in colour. Ensure those who need assistance with drinking are helped regularly. Be careful with sugar quantities in drinks, particularly for diabetic patients; opt for sugar-free options.
Consider changing menu options to cold meals with a high water content, for example fruits and salads.
Electric fans
Although fans are not recommended in clinical areas, there are certain circumstances where they may need to be used for patient/resident comfort. If they are to be used there should be a cleaning schedule in place, and not pointing the direction of a patient/resident, and should be serviced frequently. Good ventilation in a room is the priority. A risk assessment approach be taken in whatever circumstance is deemed necessary by the facility. Natural ventilation in clinical areas by opening windows and doors in so far as practical consistent with comfort and security of patients and staff; the goal is gentle air circulation rather than strong air currents.
Medications
Certain medications have increased risks during hot weather, and need to be monitored more carefully.
- Diuretics (especially loop diuretics): can lead to dehydration and electrolyte abnormalities
- Medications that interfere with cardiovascular responses such as antihypertensives and antianginal drugs
- Medications that interfere with sweating, such as anticholinergics or beta blockers
- Drugs that cause diarrhoea or vomiting, such as colchicine, antibiotics and opiates, which can lead to dehydration
- Medications that can impair renal function, such as certain antimicrobials, immunosuppressants, non-steroidal anti-inflammatories (NSAIDS), anti-ulcer agents and chemotherapies
- Agents with levels affected by dehydration, such as lithium, digoxin, antiepileptics
- Drugs that alter states of alertness, such as hypnotics, anxiolytics and analgesics
- Medications that can interfere with central nervous system thermoregulation, such as neuroleptics and serotoninergic agonists
- Drugs that increase basal metabolic rate such as thyroxine
Storage of medicines
Most medicines should be stored below 25°C and in a cool, dry place. Keep medicines out of direct sunlight, and do not leave on windowsills. Medicines should only be stored in the fridge where specified. Contact your pharmacist for further guidance.
The effects of heat on health
- Heat exhaustion, heatstroke, and other heat-related illnesses including cardiovascular and respiratory problems are a risk during the hot weather.
- The main causes of illness and death are from respiratory and cardiovascular disease – take extra care with these patients.
- Hot weather and dehydration can increase the risk of gram-negative sepsis, particularly E. coli. This risk is particularly high in the over 65 age group. It is vitally important that older people stay well hydrated to reduce this risk.
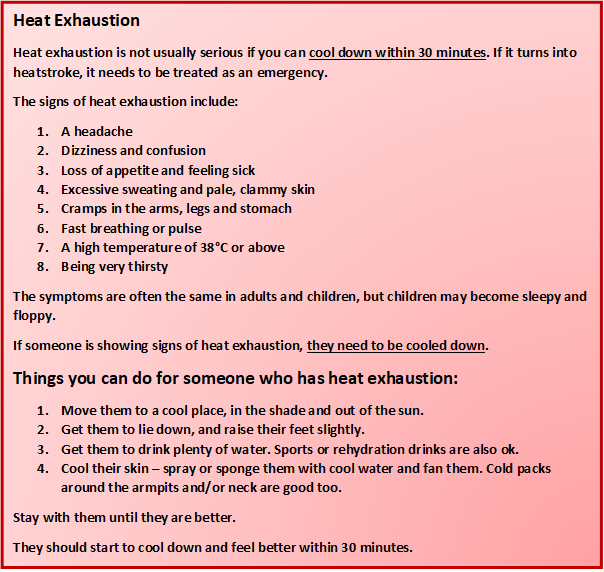
Heat-related illness can range from heat cramps, through heat exhaustion, to heatstroke. These are avoidable with good preparation and early intervention. Heat exhaustion can be managed to prevent its progression to heatstroke, which is a medical emergency.
Heat cramps may occur in the arms, legs, and stomach, and suggest electrolyte imbalance. Other physiological responses, such as sweating, are preserved at this stage of heat-related illness, and cognition is not impacted.
During heat exhaustion body temperature is rising, but the patient is still capable of dissipating heat. They will likely appear hot, flushed, and sweaty. Mild cognitive dysfunction may occur, irritability and anxiety. They might feel dizzy (dehydration, orthostatic hypotension) or uncoordinated, and nauseated. Urine output might also decrease. Heat exhaustion needs to be treated quickly to prevent progression to heatstroke.
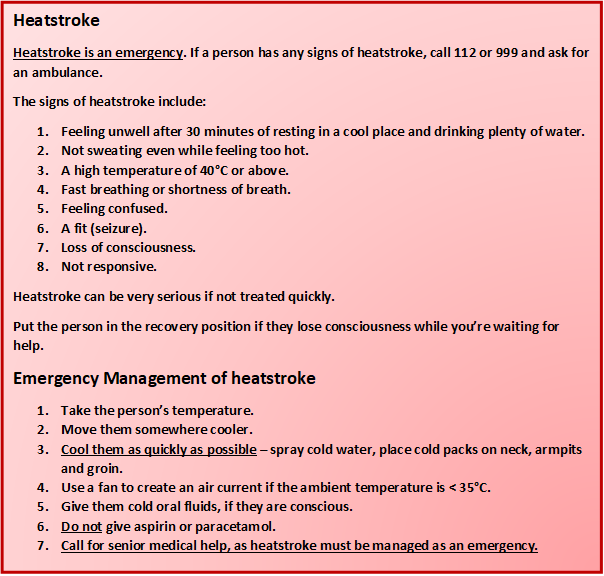
Heatstroke is a medical emergency. Urgent medical management is required to avoid serious injury and death. It is differentiated from earlier heat-related illness by the body’s loss of ability to dissipate heat and central nervous system dysfunction. It commonly presents as hyperventilation, hypotension, and shock. Failure of the thermoregulatory system means the patient can feel cool and dry. Loss of the ability to sweat is a late and severe sign and the patient can rapidly deteriorate to multiple organ failure and death.
More information can be found on the HSE and WHO websites. WHO guidelines contain more detailed management.
The boxes below detail how to recognise and manage the symptoms of heat exhaustion and heatstroke. If someone has not recovered from the symptoms of heat exhaustion after 30 minutes, or if they develop any of the signs of heatstroke, they need to be managed as an emergency.
Further Information
More information can be found on the HSE website, where there are also links to information on how to recognise and prevent heat-related illness. The National Health Protection Service of Ireland is working closely with Met Éireann to issue health alerts and advice on how to stay safe, during periods of warm weather. Updates, advice for vulnerable groups, and guidelines are published on the Health Protection Surveillance Centre website.
Created: 8 September 2023


